International Journal of Sexual and Reproductive Health Care
A study of sexual dysfunction in females having major depressive disorder
Surabhi Sharma*
Cite this as
Sharma S (2024) A study of sexual dysfunction in females having major depressive disorder. Int J Sex Reprod Health Care 7(1): 001-013. DOI: 10.17352/ijsrhc.000042Copyright Licence
© 2024 Sharma S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Introduction: Major depressive disorder has the highest lifetime prevalence of any psychiatric disorder and negatively impacts sexual functioning in many patients. Females hesitate to discuss sexual problems due to cultural barriers. So sexual dysfunctions are under-reported and under-studied.
Method: This is a cross-sectional study to evaluate the pattern of sexual dysfunction in 18 to 40-year-old married females having major depressive disorder attending psychiatry OPD in a tertiary care hospital in Delhi, India. The severity of depression was assessed by the Hamilton Depression Rating Scale (HAM-D), and sexual functioning was assessed by the Arizona Sexual Experience Scale (ASEX) and Female Sexual Function Index (FSFI) scales. Data was analysed using SPSS. Mean and standard deviation (±SD) were used to describe quantitative data meeting normal distribution. As appropriate, the chi-square or Fisher’s exact test was used to compare categorical data amongst independent groups.
Results: 64% and 56% of participants in drug naïve and on-treatment groups respectively had sexual dysfunction as per ASEX scale as compared to 10% of controls. As per the FSFI scale, 84% and 76% of participants of drug naïve and on-treatment groups had sexual dysfunction compared to 20% of the control group. Of all domains of sexual functioning, domains of desire, arousal, and orgasm were most commonly affected.
Conclusion: This study showed a high prevalence of sexual dysfunction in depressed females emphasizing the need for direct inquiry about sexual problems by the treatment provider and appropriate management for the benefit of patients.
Introduction
Major Depressive Disorder (MDD) is clinically defined as a sad mood, anhedonia, guilty feelings or low self-worth, disturbed vegetative functions like sleep and appetite, easy fatiguability, and poor concentration. In the world, around 300 million people of all age groups have depression [1]. As estimated by WHO, depression is likely to emerge as the second-largest illness in terms of morbidity in another decade in the world. As per existing data, one out of every five women, and twelve men is having depression. One of the common reasons for psychiatric referral is usually depression. The lifetime prevalence of MDD is 5% - 17% and is twice as common in females than in males [2]. The triggers for depression appear to differ, with women more often presenting with internalizing symptoms and men presenting with externalizing symptoms [3].
Depression generally leads to decreased sexual functioning [2]. In the depressed population, there is an increased risk of developing deficits in sexual functioning by 50% - 70% as compared to the non-depressed population [4-7]. All domains of the sexual cycle were disturbed in depressed females [4,5,7,8]. Montejo et al reported that symptoms like decreased libido, delay in orgasm, and anorgasmia were experienced more by depressed women in comparison to non-depressed women. Studies have also shown that antidepressants can also cause sexual dysfunctions [7,9,10]. Inter and intra-class variations were found among different antidepressants with regard to their effect on sexual functions. The presence of antidepressant treatment-emergent sexual dysfunction can notably decrease self-esteem and quality of life which creates a burden on interpersonal relations as add-on problems with comorbid depression and leading to problems of non-compliance. Sexual dysfunction of some type was reported in 26% of normal individuals, 45% of untreated depressed patients, and 63% of patients receiving treatment for depression. Increased sexual dysfunction and emotional problems may lead to an increase in associated sexual problems in patients taking treatment for depression and such treatment will not affect the libido [11]. Meta-analysis of approximately 14,000 patients showed that those with depression had a 50% to 70% risk for the development of sexual dysfunction even after comorbidities were treated [12].
Some of the meta-analyses research have compared the rate of sexual adverse effects, concluding that antidepressants cause higher sexual dysfunctions as compared to the placebo molecule with the prevalence of respective 40% and 14% [13, 14]. A few studies also showed results that 2% of patients receiving Bupropion had reported sexual arousal dysfunctions when compared to 82% of patients who were on Citalopram. The high variability in sexual dysfunction estimation may arise from various methods of assessment and the respective timing. Prospective assessment of sexual function for greater than 6 months with the application of a validated scale, reports higher rates of sexual adverse effects when compared to trial studies which mainly focused on the patient’s self-report, brief clinical assessment excluding relevant questionnaires or cross-sectional analyses. Also, antidepressant medications having major action on Serotonin (e.g., Sertraline, Citalopram, Venlafaxine) are associated with markedly higher rates of sexual dysfunction on treatment as compared to medications with predominantly noradrenergic, dopaminergic, or non-monoaminergic effects (e.g., mirtazapine, bupropion). The majority of reported adverse sexual effects in females on antidepressants were associated with sexual desire (72%) and arousal dysfunctions in the sexual cycle (83%). Approximately 42% of women receiving molecules like selective serotonin reuptake inhibitors felt the dysfunctions of orgasm.
In clinical scenarios, the onset of various symptoms of sexual adverse effects generally started to occur within about the first 3 weeks of initiation of treatment, whereas the drug’s antidepressant effects generally do not regularly appear in the initial phase of approximately 2 to 4 weeks after the initiation of management. Thus, the majority of the patients will experience disturbing sexual effects before any improvement in the mood domain of the depression [15].
Sexual function clinical assessment is required both at the initiation of clinical assessment and subsequent visits as almost half of patients who are not treated for depression also experience a disturbance in the sexual functioning [16]. Sometimes patients provide poor histories in relation to the onset of sexual adverse effects. It would be hard to know whether sexual dysfunction is mainly because of the underlying mood depression status or the iatrogenic antidepressant medication side effect without any clinical prospective assessment [17].
In some studies, it was found that 43% of women reported problems related to sexual health, among those 12% reported some related distress [18]. Sexual health issues, if causing any sort of distress, necessitate intervention. If the patient reports any sexual health problems that may be distressing, the assessment should include an evaluation of each domain of sexual response phases (i.e. desire, arousal, orgasm, pain); such assessment efficiently concluded with the help of some validated screening tool [19]. Drug classes like Phosphodiesterase Type-5 inhibitors may be helpful in treating effectively the domains of female sexual dysfunction as concluded in various meta-analyses and systemic reviews research studies [20]. Recently, Flibanserin was approved for the management of Hypoactive Sexual Desire Disorder (HSDD) in pre-menopausal women [21]. Off-label use of hormonal therapies like Oestrogen and Testosterone, are most widely employed for female sexual dysfunction.
Research in the area of sexuality is scant in India and if studied they have almost exclusively focused on male sexual dysfunction. Also, there is a lack of systematic research in India that has assessed the occurrence of sexual dysfunction in patients who are on treatment with psychotropic medications.
Review of literature
Depression and sexual dysfunction
Depression, rather than the burden of physical disease or severity of complications, is the independent factor determining the presence or absence of sexual dysfunction in women living with diabetes, multiple sclerosis, renal failure, or rheumatic disease as well as those with a history of past childhood sexual abuse [22].
The anhedonia of depression has been shown to be particularly linked to the muting of desire and response as well as to the risk of sexual pain. The most common form of chronic dyspareunia, namely Provoked Vestibulodynia (PVD), is three times more common in women with a premorbid diagnosis of depression [23].
A study done in Vellore by Singh, et al. found 77.2% in the desire domain; arousal at 91.3%, lubrication at 96.6% orgasm at 86.6% satisfaction at 81.2%% and pain at 64.4% [24].
Lauman, et al. identified the prevalence of the following categories of sexual dysfunction in depressed women as follows: low sexual desire 22%, arousal problems 14%, and sexual pain 7% [25].
McCabe, et al. concluded that the most frequent sexual dysfunctions in depressed women are desire and arousal dysfunctions [26].
Antidepressant induced sexual dysfunctions
Treatment-emergent sexual dysfunction has been reported with virtually all antidepressants. Clinical reality is that the onset of adverse sexual effects (across all phases) occurs within 1 to 3 weeks of initiating a treatment regimen, whereas the antidepressant effects do not consistently appear until approximately 2 to 4 weeks after starting a medication [27].
Rothschild in a review of research studies on antidepressants and sexual function concluded that 40% of people taking antidepressants will develop some form of sexual dysfunction [28]. Studies estimate that the incidence varies from 30% of people treated with imipramine to 25% - 73% of people treated with an SSRI [29], with 93% of the men and women treated with clomipramine in one study complaining of total or partial anorgasmia [30].
In a multicenter, prospective, Spanish study involving 1022 participants, Montejo, et al. [12] reported a 59.1% overall incidence of sexual dysfunction when all antidepressants were considered as a whole. Incidences of sexual dysfunction with SSRIs and venlafaxine (a SNRI) were high ranging between 58% and 70% – fluoxetine (57.7%), sertraline (62.9%), fluvoxamine (62.3%), venlafaxine (67%), paroxetine (70.7%), and citalopram (72.7%). This is compared with a much lower incidence for the newer 5-HT2 blockers (8% nefazodone and 24% mirtazapine). Moclobemide, a reversible MAOI, (3.9%) resulted in the lowest incidence of sexual dysfunction [31].
Montjo-Gonzales, et al. reported an overall incidence of 58% in an unblinded study involving 344 subjects who had a history of normal sexual functioning before SSRI treatments. The frequency of sexual side effects was highest for paroxetine (65%), fluvoxamine (59%), sertraline (56%) and fluoxetine (54%) [31].
Modell, et al. investigated through self-reported anonymous questionnaires, the sexual side effects of bupropion and the SSRIs (fluoxetine, paroxetine, and sertraline) among 107 outpatients. Overall, 73% of the SSRI-treated subjects reported adverse sexual side effects; in contrast, 14% of subjects were treated with Bupropion. The three SSRIs, to an equal degree, significantly decreased libido, arousal, duration of orgasm, and intensity of orgasm below levels experienced pre-morbidly. In comparison, Bupropion-treated subjects reported significant increases in libido, level of arousal, intensity of orgasm, and duration of orgasm beyond levels experienced pre-morbidly [32].
Lower rates of sexual dysfunction were reported with antidepressants like Mirtazapine, Reboxetine, Bupropion, and Moclobemide (range 0% - 24%) [33]. In a cohort study, Sexual problems of some type were found in 26% of normal subjects, 45% of non-treated depressed patients, and 63% of treated depressed patients [34].
The most commonly reported adverse sexual effects in women taking antidepressants are problems with sexual desire (72%) and sexual arousal (83%). About 42% of women taking selective Serotonin reuptake inhibitors report problems having an orgasm. Data on the effect of antidepressants on sexual pain are mixed, with some studies suggesting lubrication problems leading to pain with vaginal penetration, some reporting no effect, and still others reporting improvements in vulvodynia [35].
Patients can be hesitant to initiate a discussion regarding sexual problems for multiple reasons, including cultural differences, due to which they go undetected. For example, in the ELIXIR study, patients who were directly questioned about SD were twice as likely to report problems (69%) compared with reliance on spontaneous reports (35%). Montejo-Gonzales et al demonstrated a fourfold difference in reporting in a clinical study of 344 patients, with 58% acknowledging SD upon direct and systematic questioning, versus 14% who spontaneously reported dysfunction [11]. Different assessment methods (spontaneous report versus direct inquiry) can produce vastly different prevalence estimates.
The first step in managing antidepressant-induced sexual dysfunction is assessment which is challenging for the practitioners as taboo surrounds sex and sexual health. Although it might be awkward to discuss sexual history, making it a routine in clinics can enhance their skills and practice, transforming their awkwardness into clinical expertise, which will ensure clients are comfortable attending and can discuss issues openly. A good assessment will generate good information that will enhance effective clinical decision-making.
Materials and methods
Aim and objectives
To study and compare the pattern of sexual dysfunction in females having major depressive disorder, who are either untreated or on antidepressants and controls.
Research question
Is there any difference in the pattern of sexual dysfunction in females having major depressive disorder, who are either untreated or on antidepressants and controls?
Hypothesis
There is a difference in the pattern of sexual dysfunction in females having major depressive disorder, who are either untreated or on antidepressants and controls.
Type of study
A cross-sectional descriptive study.
Period of study
The study was conducted from November 2018 to March 2020.
Place of study
The study was conducted in the Department of Psychiatry and Drug De-Addiction Centre, Lady Hardinge Medical College, and Smt. S. K. Hospital, New Delhi.
Study population
Females between 18-40 years, fulfilling criteria for Major Depressive Disorder.
Inclusion criteria
Age group: 18 years - 40 years
Marital status: Married females
For the drug naïve group
- Diagnosed with major depressive disorder, single or recurrent episode, as per DSM-5 criteria.
- Female patients taking treatment for the first time or not taking anti-depressants for at least the last 6 months.
For females on anti-depressant
- Diagnosed with major depressive disorder, single or recurrent episode, as per DSM-5 criteria.
- On a stable dose of a single anti-depressant: Selective Serotonin Reuptake Inhibitor (SSRI), for at least 8 weeks.
For control group
- Not suffering from Major Depressive Disorder
- Accompanying the patients attending the hospital services.
Exclusion criteria
- Females having major depressive disorder with psychotic symptoms.
- Females with co-morbid psychiatric disorder (other than anxiety disorder).
- Chronic co-morbid medical illness that could cause sexual dysfunction like hypertension, diabetes, thyroid dysfunction, cardiovascular disorders(angina/MI)/ renal dysfunction, neurological disorders (stroke/spinal cord lesions), etc.
- Co-morbid diagnosis of substance dependence.
- Females who have attained menopause.
- Females that receive concurrent medications that are known to cause sexual dysfunction on a regular basis.
- Whose spouse was suffering from sexual dysfunction (based on the history) due to any causes.
Sample size and sampling technique
A total of 100 patients were selected from the depressed female patients visiting the Psychiatry OPD, and 50 were recruited in each group while following inclusion and exclusion criteria. The Purposive Sampling technique was applied.
Instruments used
- Semi-structured proforma: It was used to collect socio-demographic details of study participants.
- Modified Kuppuswamy Socio-economic Status Scale January 2018: This scale was applied to assess socio-economic status of study participants.
- Hamilton depression rating scale (17- items): This rating was applied to assess the severity of depression in patients [36].
- Arizona Sexual Experience Scale (ASEX): The ASEX scale was developed by Cynthia A. Mcgahuey, Department of Psychiatry, College of Medicine, University of Arizona. It measures 5 specific items i.e. sexual drive, arousal, vaginal lubrication, ability to reach orgasm, and satisfaction from orgasm. This is a 6-point Likert scale ranging from hyperfunction (1) to hypofunction (6). A total ASEX score of ≥ 19, one item with a score of ≥ 5, or any three items with a score of ≥ 4 indicate sexual dysfunction. It can be used in heterosexual or homosexual populations, regardless of the availability of sexual partners [37]. It is a self-rated as well as clinician-rated scale and is available in the English language. It takes less than 5 minutes to complete the application. It has excellent internal consistency and scale reliability (alpha = 0.9055). The scale consists of strong test-retest reliability (for patients, r = 0.801, p < 0.01; for controls, r = 0.892, p < 0.01) [38]. It is available freely without any copyrights.
- Female sexual function index (FSFI): The scale was developed by Raymond Rosen, Ph.D., USA. It is a 19-item questionnaire. This is a multi-dimensional self-report instrument for the assessment of the key dimensions of sexual functioning in women in the last 1 month. The scale has 6 domains, namely: desire (2 questions), subjective arousal (4 questions), lubrication (4 questions), orgasm (3 questions), satisfaction (3 questions) and pain (3 questions). The overall test-retest reliability coefficients are high for each of the individual domains (r = 0.79 to 0.86), high degree of internal consistency (Cronbach’s alpha values of 0.82 and higher), and good construct validity [39]. FSFI score of < 26.55 indicates sexual dysfunction. The cut-off scores for sexual dysfunction in various domains are < 4.28 for sexual desire, < 5.08 for arousal, < 5.45 for lubrication, < 5.05 for orgasm, < 5.04 for the satisfaction and < 5.51 for the domain of pain [40]. The scale is freely available in English and translated into Hindi language.
Procedure
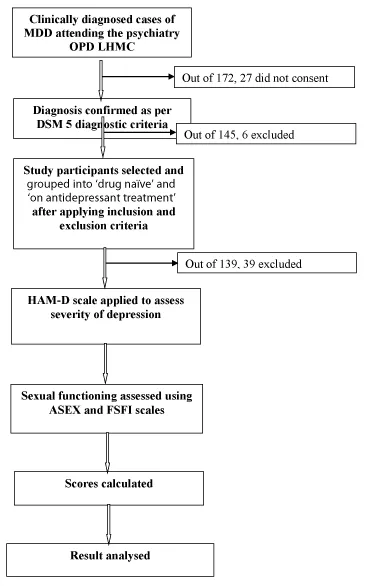
All female patients fulfilling the diagnosis of MDD as per DSM 5 diagnostic criteria were evaluated on inclusion and exclusion criteria and those fulfilling the same were approached for participation in the study. The study protocol was explained with a patient information sheet (appendix 2) and those who gave written informed consent (appendix 1) were recruited. Socio-demographic data and clinical data were recorded using a Semi-Structured Proforma and Modified Kuppuswamy Socio-Economic Scale. They were assessed on the Hamilton Depression Rating Scale 17 items for severity of depression. Sexual dysfunction was assessed using ASEX and FSFI scales. The control group of women was recruited as per inclusion and exclusion criteria after taking written informed consent and assessed on ASEX and FSFI scales. Those who were found to have sexual dysfunction as per ASEX or FSFI were informed about the same and offered intervention. These findings were then assessed and interpreted (Figure 1).
Outcome variables
- A score of the Hamilton depression rating scale (HAM D) for the severity of depression.
- Scores of Arizona sexual experience scale (ASEX), female sexual function index (FSFI), domain score, and overall score.
- Correlation of the above scores.
Statistical methods
- Data so generated after the application of the HAM-D scale and calculating scores of ASEX and FSFI was entered and analyzed using computer-based software (SPSS v25.0)
- Descriptive statistics were used for sociodemographic variables.
- Chi-square and Fisher exact tests were carried out to test for significance.
- p-value of less than 0.05 was considered statistically significant.
Results
- Sociodemographic characteristics of study population
- Characteristics of depression in the study population
- Sexual functioning in the study population
- Correlation of sexual functioning with severity of depression
Sociodemographic characteristics of study population
Age: As depicted in the table, the mean ages in drug naïve, treatment, and control groups were 33.84, 35.22, and 31.42 years respectively. There was a significant difference between the control versus drug naïve and treatment group in terms of age with a p - value being < 0.05 whereas no significant difference was found between drug naïve and treatment groups (p – value > 0.05) (Table 1).
Education: As depicted in the table, the majority of participants were educated up to the 10th standard i.e. 78% in drug naïve and 74% in the treatment group. There was a significant difference between the various groups in terms of the distribution of education (X^2 = 13.547, p = 0.001) (Table 2).
Occupation: As depicted in the table, 82% of participants were unemployed in the drug naïve group and 86% were unemployed in the treatment group. There was a significant difference between the various groups in terms of the distribution of occupation (X^2 = 19.108, p = < 0.001) (Table 3).
Head of family: As depicted in the table, the majority i.e. 94% of participants in drug naïve and 84% in the treatment group had ‘husbands’ as the head of the family. There was no significant difference between the various groups in terms of the distribution of Head of Family (X^2 = 7.486, p = 0.130) (Table 4).
Type of family: As depicted in the table, 80% of participants in the drug naïve and 72% in the treatment group belonged to the nuclear family. There was no significant difference among the various groups in terms of the distribution of Type of Family (X^2 = 4.889, p = 0.299) (Table 5).
Religion: As per the table majority of participants belonged to the Hindu religion with 66% in drug naïve and 70% in the treatment group. There was no significant difference between the various groups in terms of the distribution of Religion (X^2 = 7.437, p = 0.340) (Table 6).
Residence: The majority i.e. 92%participants in drug naïve and 96% in the treatment group belonged to urban areas and there was no significant difference between various groups in terms of distribution of residence (Table 7).
Socio- economic status: The majority of the participants i.e. 50% and 52% respectively in the drug-naive and treatment group belonged to the middle socio-economic class followed by the lower class. A significant difference has been observed between the various groups in terms of the distribution of Socio-Economic Status (X^2 = 9.701, p = 0.024) (Table 8).
Characteristics of depression in the study population
Score of Hamilton Depression Rating Scale (HAM-D): The mean HAM-D score in drug naïve, on treatment and control group was 19.2, 16.2, and 1.3 respectively. There was no significant difference between the Drug naïve and the treatment group in terms of HAM-D score with a p-value being 0.117 (Table 9).
Severity of depression: It is observed that the majority of the participants (56%) in the drug naïve group had moderate depression whereas 50% of participants on treatment had mild depression and 46% had moderate severity (Table 10).
Sexual functioning in study groups
Sexual functioning using ASEX scale: There was a significant difference between the control group versus drug naïve and treatment groups in terms of ASEX: domain score as well as total score; with p-value being < 0.05 (Table 11).
Score interpretation of the ASEX scale: In the study, as per the criteria of ASEX one item score >5, sexual dysfunction was present in 68% of drug naïve participants, 64% of participants of the treatment group, and 8% of participants of the control group. The difference was statistically significant between the control group versus the drug naïve and treatment group (Table 12).
In the study, as per the criteria of ASEX total score >19, sexual dysfunction was present in 64% of drug naïve depressed females, 56% of depressed currently on SSRI treatment, and 10% control population. The difference was statistically significant when both drug naïve and the treatment groups were compared with controls whereas no statistically significant difference was present between drug naïve and treatment groups (Table 13).
Sexual functioning using female sexual functioning index (FSFI) scale
There was a significant difference between each of the domain scores and the total score of the FSFI scale when a comparison of the drug naïve and on-treatment group was made with a control group with p - value <0.05 but no such significant difference was noted when these 2 groups were compared with each other (as p - value >0.05) (Table 14).
Score interpretation of FSFI scale: A score of <4.28 in the desire domain depicts sexual dysfunction in this domain. As per this cut-off, Sexual dysfunction was present in 94% of participants in the drug naïve group and in 96% participants of treatment group in contrast to 46% of controls. The difference was significant when drug naïve and treatment groups were compared to controls, but no statistically significant difference was found when the two groups were compared with each other (Table 15).
Sexual dysfunction in the domain of arousal was present in 92% of participants of the drug naïve group and in 86% of participants of the treatment group in contrast to 30% of controls. The relationship was significant when drug naïve and treatment groups were compared to controls, but no statistically significant difference was found when the two groups were compared with each other (Table 16).
Sexual dysfunction in the domain of lubrication was present in 84% of participants in each of the drug naïve group and treatment group in contrast to 42% of controls. The difference was statistically significant between the controls and depressed group (both drug naïve and on treatment) (Table 17).
Sexual dysfunction in the domain of orgasm was present in 90% of participants of the drug naïve group and in 92% of participants of the treatment group in contrast to 40% of controls. The difference was statistically significant between the controls and depressed group (both drug naïve and on treatment) (Table 18).
Considering the score cut-off, sexual dysfunction in the domain of arousal was present in 86% of participants of the drug naïve group and in 80% of participants of the treatment group in contrast to 44% of controls. The difference was statistically significant between the controls and depressed group (both drug naïve and on treatment) (Table 19).
Considering the score cut-off, sexual dysfunction in the domain of pain was present in 64% of participants of the drug naïve group and in 50% of participants of the treatment group in contrast to 16% of controls. The difference was statistically significant between the controls and depressed group (both drug naïve and on treatment) (Table 20).
Considering the total score cut-off, sexual dysfunction was present in 84% of participants of the drug naïve group and in 76% of participants of the treatment group in contrast to 20% of controls. The difference was statistically significant between the controls and depressed group (both drug naïve and on treatment) (Table 21).
Correlation of severity of depression with sexual dysfunction
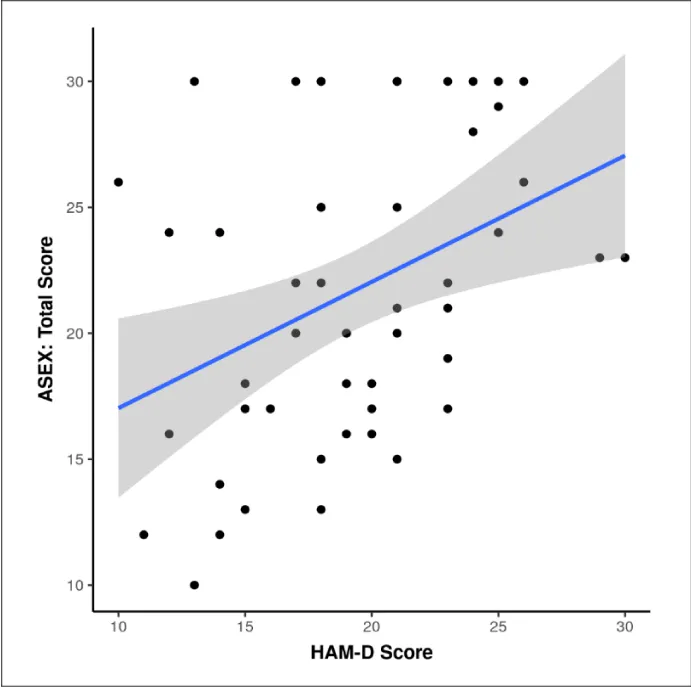
Correlation between severity of depression and sexual dysfunction in drug naïve participants as per ASEX scale: Out of the 32 participants having sexual dysfunction in the drug naïve group, 4 had mild depression, which was 30.8% of the total participants having mild depression; 19 had moderate (67.9% of total moderately depressed), and 9 had severe depression (100% of the total severely depressed) (Figure 2)(Table 22).
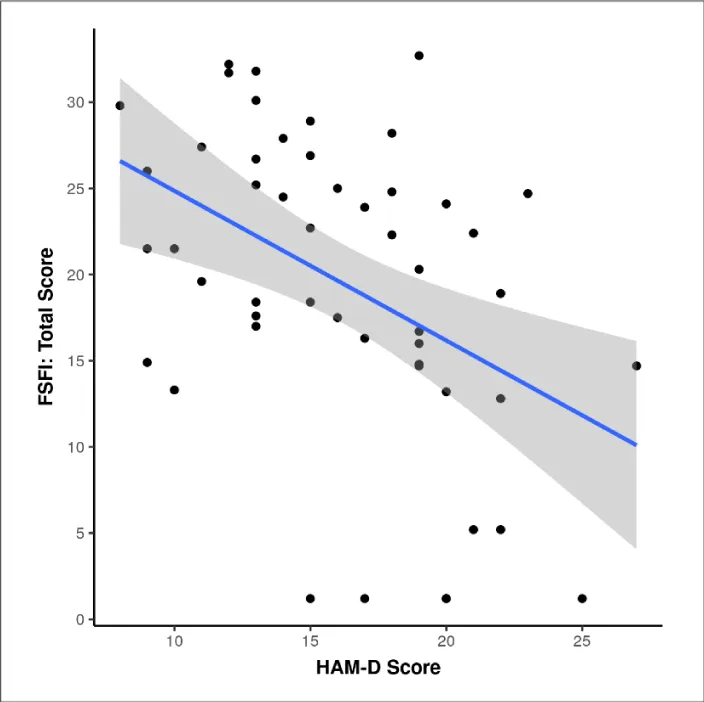
Spearman’s correlation between the two variables was 0.39, which was statistically significant at a p-value of 0.006, implying that sexual dysfunction increases with increasing severity of depression (Figure 3).
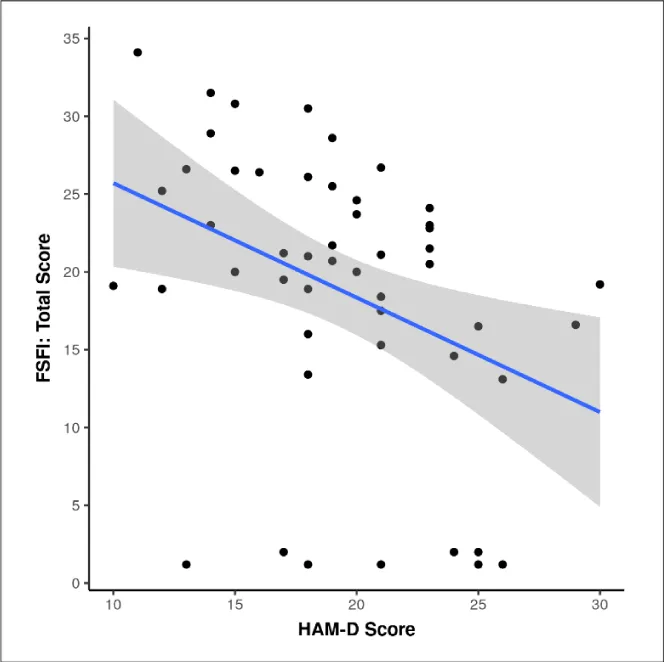
Correlation between severity of depression and sexual dysfunction in drug naïve participants as per FSFI scale: The table shows the association between the FSFI score and the HAM D severity score. The percentage of participants having sexual dysfunction increased with increasing severity of depression. The difference was statistically significant for the domain of lubrication and pain as well as for total score (Table 23).
The Spearman correlation between the two variables was -0.42, which was statistically significant at a p - value of 0.002, implying that sexual dysfunction increases with increasing severity of depression.
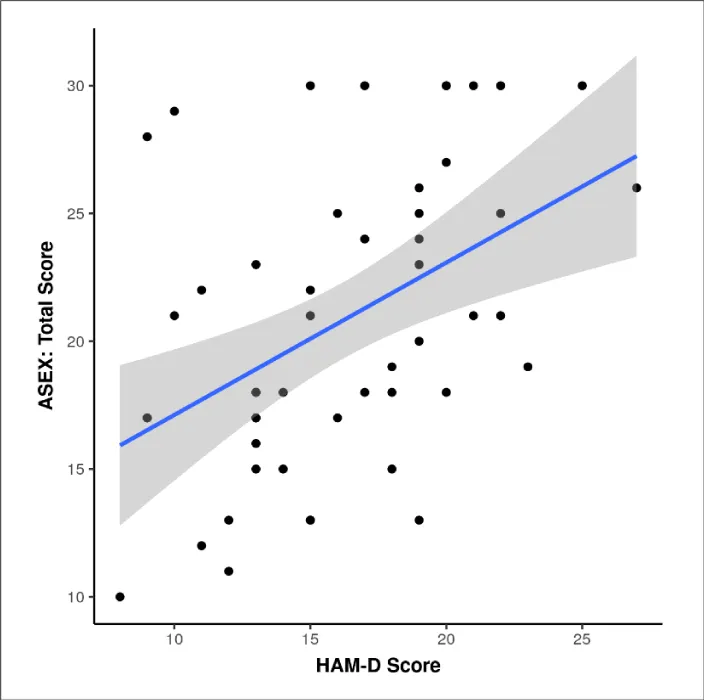
Association between severity of depression and sexual dysfunction in drug treatment participants as per ASEX scale: Out of the 28 participants having sexual dysfunction in the drug naïve group, 9 had mild depression, which was 36% of the total participants having mild depression; 17 had moderate (73.9% of total moderately depressed), and 2 had severe depression (100% of the total severely depressed) (Table 24).
Spearman correlation between the two variables was 0.49, which was statistically significant at p-value <0.001, implying that sexual dysfunction increases with increasing severity of depression (Figure 4).
Association between severity of depression and sexual dysfunction in drug treatment groups per FSFI scale: The table shows the association between sexual dysfunction as per FSFI score and HAM D severity score. The percentage of participants having sexual dysfunction increased with increasing severity of depression, except for the domain of desire (Table 25).
Spearman correlation between the two variables was -0.45, which was statistically significant at p - value < 0.001, implying that sexual dysfunction increases with increasing severity of depression (Figure 5).
Discussion
The study was carried out at a tertiary care hospital situated in an urban area to assess the pattern of sexual dysfunction in females having major depressive disorder in ‘drug naïve’ and ‘on antidepressant’ groups. The study included 50 participants each in ‘drug naïve depressed’, ‘on treatment depressed’ females, and controls and they were assessed using the HAM- D scale for severity of depression and ASEX and FSFI scales for sexual functioning. The results obtained are discussed as follows.
Sociodemographic variables
In the current study, the mean age of treatment-naïve depressed females was 33.84 years and that of depressed females on treatment was 35.22 years, with a majority of the cases being within the age group of 30 years - 40 years in both groups. In India, a study conducted by Reddy, et al. [41] and Kendurkar, et al. [42] reported similar results with the mean age being 32 years and 35 years respectively.
Most of the subjects i.e. 78% in drug-naïve, 86%in treatment, and 66% in the control group belonged to the age group of 30 years - 40 years at the time of presentation
With respect to education, we concluded that 66% of the participants belonging to depressed groups (both ‘drug naïve’ and ‘on treatment’) were educated up to the 10th standard whereas the majority of controls were educated above the 10th standard, which is similar to results shown by Sreelakshmy, et al. 2017 [5], wherein 70% of the cases were educated upto High School & 10% had higher education; similar findings shown by Niteen Abhivant [43].
It emerged from the study that > 80% of depressed groups were unemployed, whereas this figure was 54% in the control group suggesting depression was more prevalent in the unemployed group 82% of the participants were unemployed in the drug naïve group and 86% were unemployed in the treatment group. Similar results were concluded by Sreelakshmy, et al. [5] having 90% of cases unemployed and Reddy, et al. [41] with 54% of cases being unemployed.
The present study showed that the maximum number of participants i.e. 80% in the drug naïve and 70% in the treatment group belonged to nuclear families. Similar results were reported in a study conducted by Kourgulzar and Bhat 2018 [44], where depression was more prevalent in nuclear families i.e. 63.4 %.
In this study >90% of participants resided in urban areas. The study conducted by Arvind, et al. 2019 [45] also reported depression is more common in urban dwellers. The findings of our study may be a reflection of the population catered by hospitals rather than the distribution of depression itself.
In our study, ~46% of participants in the depressed group (both ‘on treatment’ and ‘drug naïve’) belonged to lower socio-economic status as compared to 24% of controls belonging to lower socio-economic status. This is comparable to studies conducted by Mathias, et al. 2015 [46] and Arvind, et al. 2019 [45] which reported depression to be more prevalent in lower socio-economic status.
Characteristics of depression in the study population
The average duration of illness in a Drug-Naive depressed female was 7.7 months and in the ‘On-Treatment’ group was nearly 12 months.
In this study, the mean HAM- D score in the ‘Drug-Naive’ group was 19.29 (+ 4.62), with 30 being the highest score and 10 being the lowest score. The mean score in the ‘On-Treatment’ group was 16.18 (+ 4.48), with 27 being the highest score and 8 being the lowest. This was comparable to the study conducted by Roy et al [7] wherein the mean HAM- D score in treatment naïve depressed females was reported to be 19.13. Another study conducted by Reddy et al., on depressed females, both with and without treatment, had a HAM-D score of 14.6.
The majority (56%) of participants in the ‘Drug-Naive’ group had moderate depression whereas in the ‘On Treatment’ group 50% had mild depression and 46% had moderate depression.
In this study, no statistical relationship was found between the severity of depression and demographic variables like education, occupation, residential area, and type of family.
Sexual functioning in study groups
In this study, sexual functioning was assessed in all the groups, using ASEX and FSFI scales.
The mean domain as well as the total ASEX score was more in ‘Drug-Naive’ and ‘On Treatment’ group than in the ‘Control’ group and the difference was statistically significant. As per the total score criteria, Sexual Dysfunction was present in 64% and 56% of subjects in ‘Drug-Naive’ and ‘On-Treatment’ groups respectively while only 10% of the subjects from the ‘Control’ group had Sexual Dysfunction. The finding of the study was consistent with the study done by Roy et al [7], who reported that on the ASEX scale, 73.3% of participants in the Depressed group had Sexual Dysfunction whereas it was only 20% in the ‘Control’ group. Similar results were also demonstrated in the study conducted by Reddy, et al. [41]; wherein a greater proportion of subjects in the Depressed group had Sexual Dysfunction than the ‘Control’ group and the difference was statistically significant.
When assessed using the FSFI scale, the mean domain and total scores were comparable in both ‘drug naïve’ and ‘on treatment’ groups; with minimum scores in the domains of orgasm and desire in both the groups. The difference in scores between the depressed subjects and the control group was statistically significant with a p - value being <0.001.
When interpreting the total scores, sexual dysfunction was present in 84% of ‘drug naïve’ and 76% of subjects in the ‘treatment’ group whilst only 20% of controls had SD. This finding was comparable to studies conducted by Roy, et al. [7] and Abhivant and Sawant [43] who reported SD to be present in 70% and 67% of drug naïve depressed females respectively. Another study by Sreelakshmy, et al. reported SD to be present in 90% of study participants, though it quoted a smaller sample size as a possible reason for the higher prevalence of SD in their study. A study conducted by Reddy, et al. reporting a 40% prevalence of SD explained overrepresentation of the mild and moderate depressive cases in their study sample as a probable reason for the slightly lower FSD in both ASEX and FSFI.
In our study, the maximum number of subjects had dysfunction in the domain of desire (94% in drug naïve and 96% in ‘treatment’ groups) followed by orgasm and arousal. A study conducted by Thakurta, et al. reported majority of subjects had dysfunction in domains of arousal and orgasm [47]. The study conducted by Reddy et al., found SD to be reported more in lubrication, pain, and orgasm domains though all components of sexual functioning were affected.
Correlation of sexual functioning with severity of depression
The present study found a significant positive correlation between HAM-D and ASEX total scores in both ‘Drug-Naive’ (rho = 0.39, p = 0.006) and ‘On-Treatment’ (rho = 0.49, p = <0.001) groups of depressed females.
A study conducted by Thakurta, et al. [47] reported a positive correlation between HAM- D scores and ASEX scores, though their study had a strong correlation (r = 0.817, p < 0.000); whereas our study found a moderate correlation between the variables.
Another study conducted by Muzawar, et al. [48] also reported a positive correlation between ASEX scores and HAM-D in Drug-Naive subjects which was significant.
The scatterplot between HAM-D and FSFI total scores depicted a significant negative correlation in both “drug naïve” (rho = -0.42, p = 0.002) and “on treatment” (rho = -0.45, p = < 0.001) depressed females; Similar trends were observed when domain wise depiction of FSFI scale was done across HAM-D, suggesting poorer sexual functioning with increasing severity of depression. These findings were similar to the study conducted by Muzawar, et al. [48] who reported a negative correlation between HAM-D and FSFI scores in depressed females, both drug naïve and on antidepressants.
Limitations
The cross-sectional design of the study can only help in obtaining associations between the different study variables. It cannot establish a causal relationship for which a longitudinal study design will be more appropriate.
Our sample size was relatively small which might have caused the lack of significant differences in relation to some variables.
The sample size was conveniently selected considering the patient population at the centre of the study and the duration of the study. A larger, more appropriately calculated sample size can increase the power of the study.
The sample was drawn from a clinical population; therefore, the community prevalence of the study variables cannot be estimated.
Stressful life events were not considered in this study which could have affected the sexual functioning or other variables.
Conclusion
The study attempted to assess the pattern of sexual dysfunction and dyadic adjustment in females having major depressive disorder, meeting the diagnostic criteria of DSM 5 and inclusion and exclusion criteria of the study, one group being drug naïve and the other one on antidepressants.
The hypothesis at the beginning of this study was that there is a difference in the pattern of sexual dysfunction in females having major depressive disorder who are either untreated or on antidepressants and controls. It was found that sexual dysfunction was significantly higher in depressed females as compared to controls but no difference was found between the untreated and ‘on treatment’ groups.
Sexual dysfunction was present in 64% of drug naïve and 56% of females on antidepressants compared to 10% in control according to the ASEX scale. When compared according to the FSFI scale 84% drug naïve, 76% on antidepressants had sexual dysfunction compared to 20% control. Thus, suggesting that ASEX and FSFI are equally good tools for determining sexual dysfunction. The study also suggests that all the domains of sexual functioning namely desire, arousal, lubrication, orgasm, satisfaction, and pain were adversely affected in depressed females of which desire, followed by orgasm and arousal were affected the most. There was no significant difference in sexual functioning between the drug naïve and treatment group in the current study. The study also found a significant correlation between ASEX and HAM- D scores, FSFI and HAM-D scores suggesting poorer sexual functioning with increasing severity of depression.
The study also indicated a poorer dyadic adjustment in both the groups of depressed females compared to the control group. A significant negative correlation was found between dyadic adjustment and severity of depression in both ‘drug naïve’ and ‘on treatment’ groups of depressed females suggesting that marital distress increased with increasing severity of depression.
The study also found that most of the depressed females belonged to lower educational and social backgrounds and were unemployed which was significantly higher when compared to controls
The study will further the understanding of the high prevalence of sexual dysfunction in depressed females while emphasizing the inquiry about sexual dysfunction in depressed patients. It also impresses upon the requirement or awareness of various aspects of sexuality and the need for education for early detection and treatment of sexual dysfunction in depressed females.
Since due to social taboos the patients may not come out openly with such issues on their own, it is pertinent to ask about sexual problems in depressed females and treat them accordingly so that the patients improve optimally.
Hence, the medical practitioners need to explore the problems of the female patients to assess the female sexual needs and functions ensuring privacy and confidentiality using standard rating scales which can further aid in better appreciation regarding treatment and drug selection.
Future directions
- Studies with a larger sample size may be conducted to replicate and expand the findings of this study.
- Similar studies including the unmarried sexually active depressed females may also be conducted.
- Longitudinal studies may be planned with periodic assessments of sexual functioning and assess their evolution with the course of the disorder.
- Studies comparing the effects of different classes of antidepressant drugs on sexual functioning in depressed females may be done.
- Depression. World Health Organization. 2018. http://www.who.int/news-room/fact-sheets/detail/depression
- Sadock B, Sadock V, Ruiz P, Kaplan H. Kaplan & Sadock's comprehensive textbook of psychiatry. Philadelphia, Pa. Lippincott Williams & Wilkins. 2009.
- Bartels M, Cacioppo JT, van Beijsterveldt TC, Boomsma DI. Exploring the association between well-being and psychopathology in adolescents. Behav Genet. 2013 May;43(3):177-90. doi: 10.1007/s10519-013-9589-7. Epub 2013 Mar 8. PMID: 23471543; PMCID: PMC3897864.
- Kendler KS, Gardner CO. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. American Journal of Psychiatry. 2014; 171(4):426-35.
- Sreelakshmy K, Velayudhan R, Kuriakose D, Nair R. Sexual dysfunction in females with depression: a cross-sectional study. Trends Psychiatry Psychother. 2017 Apr-Jun;39(2):106-109. doi: 10.1590/2237-6089-2016-0072. PMID: 28700039.
- Thakurta RG, Singh OP, Bhattacharya A, Mallick AK, Ray P, Sen S, Das R. Nature of sexual dysfunctions in major depressive disorder and its impact on quality of life. Indian J Psychol Med. 2012 Oct;34(4):365-70. doi: 10.4103/0253-7176.108222. PMID: 23723546; PMCID: PMC3662135.
- Roy P, Manohar S, Raman R, Sathyanarayana Rao TS, Darshan MS. Female sexual dysfunction: A comparative study in drug naive 1(st) episode of depression in a general hospital of South Asia. Indian J Psychiatry. 2015 Jul-Sep;57(3):242-8. doi: 10.4103/0019-5545.166623. PMID: 26600576; PMCID: PMC4623641.
- Atlantis E, Sullivan T. Bidirectional association between depression and sexual dysfunction: a systematic review and meta-analysis. J Sex Med. 2012 Jun;9(6):1497-507. doi: 10.1111/j.1743-6109.2012.02709.x. Epub 2012 Mar 29. PMID: 22462756.
- Mathew RJ, Weinman ML. Sexual dysfunctions in depression. Arch Sex Behav. 1982 Aug;11(4):323-8. doi: 10.1007/BF01541593. PMID: 7149967.
- Williams K, Reynolds MF. Sexual dysfunction in major depression. CNS Spectr. 2006 Aug;11(8 Suppl 9):19-23. doi: 10.1017/s1092852900026729. PMID: 16871134.
- Kennedy SH, Rizvi S. Sexual dysfunction, depression, and the impact of antidepressants. J Clin Psychopharmacol. 2009 Apr;29(2):157-64. doi: 10.1097/JCP.0b013e31819c76e9. PMID: 19512977.
- Angst J. Sexual problems in healthy and depressed persons. Int Clin Psychopharmacol. 1998 Jul;13 Suppl 6:S1-4. doi: 10.1097/00004850-199807006-00001. PMID: 9728667.
- Bonierbale M, Lançon C, Tignol J. The ELIXIR study: evaluation of sexual dysfunction in 4557 depressed patients in France. Curr Med Res Opin. 2003;19(2):114-24. doi: 10.1185/030079902125001461. PMID: 12740155.
- Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009 Jun;29(3):259-66. doi: 10.1097/JCP.0b013e3181a5233f. PMID: 19440080.
- Reichenpfader U, Gartlehner G, Morgan LC, Greenblatt A, Nussbaumer B, Hansen RA, Van Noord M, Lux L, Gaynes BN. Sexual dysfunction associated with second-generation antidepressants in patients with major depressive disorder: results from a systematic review with network meta-analysis. Drug Saf. 2014 Jan;37(1):19-31. doi: 10.1007/s40264-013-0129-4. PMID: 24338044.
- Gelenberg AJ, Dunner DL, Rothschild AJ, Pedersen R, Dorries KM, Ninan PT. Sexual functioning in patients with recurrent major depressive disorder enrolled in the PREVENT study. J Nerv Ment Dis. 2013 Apr;201(4):266-73. doi: 10.1097/NMD.0b013e318288d298. PMID: 23538970.
- Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008 Nov;112(5):970-8. doi: 10.1097/AOG.0b013e3181898cdb. PMID: 18978095.
- Johannes CB, Clayton AH, Odom DM, Rosen RC, Russo PA, Shifren JL, Monz BU. Distressing sexual problems in United States women revisited: prevalence after accounting for depression. J Clin Psychiatry. 2009 Dec;70(12):1698-706. doi: 10.4088/JCP.09m05390gry. PMID: 20141709.
- Segraves RT, Balon R. Antidepressant-induced sexual dysfunction in men. Pharmacol Biochem Behav. 2014 Jun;121:132-7. doi: 10.1016/j.pbb.2013.11.003. Epub 2013 Nov 15. PMID: 24239785.
- McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, Manber R. The Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther. 2000 Jan-Mar;26(1):25-40. doi: 10.1080/009262300278623. PMID: 10693114.
- Sang JH, Kim TH, Kim SA. Flibanserin for Treating Hypoactive Sexual Desire Disorder. J Menopausal Med. 2016 Apr;22(1):9-13. doi: 10.6118/jmm.2016.22.1.9. Epub 2016 Apr 26. PMID: 27152308; PMCID: PMC4854663.
- Maiorino MI, Bellastella G, Castaldo F, Petrizzo M, Giugliano D, Esposito K. Sexual function in young women with type 1 diabetes: the METRO study. J Endocrinol Invest. 2017 Feb;40(2):169-177. doi: 10.1007/s40618-016-0542-5. Epub 2016 Sep 9. PMID: 27613610.
- Khandker M, Brady SS, Vitonis AF, Maclehose RF, Stewart EG, Harlow BL. The influence of depression and anxiety on risk of adult onset vulvodynia. J Womens Health (Larchmt). 2011 Oct;20(10):1445-51. doi: 10.1089/jwh.2010.2661. Epub 2011 Aug 8. PMID: 21823918; PMCID: PMC3186444.
- Singh JC, Tharyan P, Kekre NS, Singh G, Gopalakrishnan G. Prevalence and risk factors for female sexual dysfunction in women attending a medical clinic in south India. J Postgrad Med. 2009 Apr-Jun;55(2):113-20. doi: 10.4103/0022-3859.52842. PMID: 19550056.
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999 Feb 10;281(6):537-44. doi: 10.1001/jama.281.6.537. Erratum in: JAMA 1999 Apr 7;281(13):1174. PMID: 10022110.
- McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, Laumann E, Lee SW, Segraves RT. Incidence and Prevalence of Sexual Dysfunction in Women and Men: A Consensus Statement from the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016 Feb;13(2):144-52. doi: 10.1016/j.jsxm.2015.12.034. PMID: 26953829.
- Gelenberg AJ, Dunner DL, Rothschild AJ, Pedersen R, Dorries KM, Ninan PT. Sexual functioning in patients with recurrent major depressive disorder enrolled in the PREVENT study. J Nerv Ment Dis. 2013 Apr;201(4):266-73. doi: 10.1097/NMD.0b013e318288d298. PMID: 23538970.
- Rothschild AJ. Sexual side effects of antidepressants. J Clin Psychiatry. 2000;61 Suppl 11:28-36. PMID: 10926052.
- Kennedy SH, Eisfeld BS, Dickens SE, Bacchiochi JR, Bagby RM. Antidepressant-induced sexual dysfunction during treatment with moclobemide, paroxetine, sertraline, and venlafaxine. J Clin Psychiatry. 2000 Apr;61(4):276-81. doi: 10.4088/jcp.v61n0406. PMID: 10830148.
- Montejo AL, Llorca G, Izquierdo JA, Rico-Villademoros F. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62 Suppl 3:10-21. PMID: 11229449.
- Montejo-González AL, Llorca G, Izquierdo JA, Ledesma A, Bousoño M, Calcedo A, Carrasco JL, Ciudad J, Daniel E, De la Gandara J, Derecho J, Franco M, Gomez MJ, Macias JA, Martin T, Perez V, Sanchez JM, Sanchez S, Vicens E. SSRI-induced sexual dysfunction: fluoxetine, paroxetine, sertraline, and fluvoxamine in a prospective, multicenter, and descriptive clinical study of 344 patients. J Sex Marital Ther. 1997 Fall;23(3):176-94. doi: 10.1080/00926239708403923. PMID: 9292833.
- Modell JG, Katholi CR, Modell JD, DePalma RL. Comparative sexual side effects of bupropion, fluoxetine, paroxetine, and sertraline. Clin Pharmacol Ther. 1997 Apr;61(4):476-87. doi: 10.1016/S0009-9236(97)90198-3. PMID: 9129565.
- Clayton AH, Croft HA, Handiwala L. Antidepressants and sexual dysfunction: mechanisms and clinical implications. Postgrad Med. 2014 Mar;126(2):91-9. doi: 10.3810/pgm.2014.03.2744. PMID: 24685972.
- Clayton AH, Campbell BJ, Favit A, Yang Y, Moonsammy G, Piontek CM, Amsterdam JD. Symptoms of sexual dysfunction in patients treated for major depressive disorder: a meta-analysis comparing selegiline transdermal system and placebo using a patient-rated scale. J Clin Psychiatry. 2007 Dec;68(12):1860-6. doi: 10.4088/jcp.v68n1205. PMID: 18162016.
- Angst J. Sexual problems in healthy and depressed persons. Int Clin Psychopharmacol. 1998 Jul;13 Suppl 6:S1-4. doi: 10.1097/00004850-199807006-00001. PMID: 9728667.
- HAMILTON M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960 Feb;23(1):56-62. doi: 10.1136/jnnp.23.1.56. PMID: 14399272; PMCID: PMC495331.
- McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, Manber R. The Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther. 2000 Jan-Mar;26(1):25-40. doi: 10.1080/009262300278623. PMID: 10693114.
- McGahuey CA, Delgado PL, Gelenberg AJ. Assessment of sexual dysfunction using the Arizona sexual experiences scale (ASEX) and implications for the treatment of depression. Psychiatric annals. 1999; 29(1):39-45.
- Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D'Agostino R Jr. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000 Apr-Jun;26(2):191-208. doi: 10.1080/009262300278597. PMID: 10782451.
- Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005 Jan-Feb;31(1):1-20. doi: 10.1080/00926230590475206. PMID: 15841702.
- Reddy RM, Saravanan RA, Praharaj SK, Thirunavukarasu M. Sexual Dysfunction in Women with Depression: A Hospital-Based Cross-sectional Comparative Study. Indian J Psychol Med. 2020 Jan 6;42(1):46-51. doi: 10.4103/IJPSYM.IJPSYM_321_19. PMID: 31997865; PMCID: PMC6970310.
- Kendurkar A, Kaur B. Major depressive disorder, obsessive-compulsive disorder, and generalized anxiety disorder: do the sexual dysfunctions differ? Prim Care Companion J Clin Psychiatry. 2008;10(4):299-305. doi: 10.4088/pcc.v10n0405. PMID: 18787674; PMCID: PMC2528235.
- Abhivant N, Sawant N. Sexual dysfunction in depressed Indian women attending a hospital out-patient department in Mumbai. Sri Lanka Journal of Psychiatry. 2013; 2:4(1).
- KourGulzar P, Bhat A. Assessing Prevalence of Depression Among General Population of Selected Rural Community-A Descriptive Survey Design. Journal of Psychiatry. 2018; 21(3).
- Arvind BA, Gururaj G, Loganathan S, Amudhan S, Varghese M, Benegal V, Rao GN, Kokane AM, B S C, P K D, Ram D, Pathak K, R K LS, Singh LK, Sharma P, Saha PK, C R, Mehta RY, T M S; NMHS collaborators group. Prevalence and socioeconomic impact of depressive disorders in India: multisite population-based cross-sectional study. BMJ Open. 2019 Jun 27;9(6):e027250. doi: 10.1136/bmjopen-2018-027250. PMID: 31253618; PMCID: PMC6609075.
- Mathias K, Goicolea I, Kermode M, Singh L, Shidhaye R, Sebastian MS. Cross-sectional study of depression and help-seeking in Uttarakhand, North India. BMJ Open. 2015 Nov 20;5(11):e008992. doi: 10.1136/bmjopen-2015-008992. PMID: 26589428; PMCID: PMC4663438.
- Thakurta RG, Singh OP, Bhattacharya A, Mallick AK, Ray P, Sen S, Das R. Nature of sexual dysfunctions in major depressive disorder and its impact on quality of life. Indian J Psychol Med. 2012 Oct;34(4):365-70. doi: 10.4103/0253-7176.108222. PMID: 23723546; PMCID: PMC3662135.
- Mujawar S, Chaudhury S, Saldanha D. Sexual Dysfunction in Women with Depressive Disorder: A Prospective, Hospital Based Study. Journal of Psychosexual Health. 2019; 1(2):129-39.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
