International Journal of Sexual and Reproductive Health Care
Dutch Sexologist perceptions on monitoring nocturnal erectile function
Evelien J Trip1-3*, Melianthe P Nicolai4,5, Henk W Elzevier3, Rob CM Pelger3 and Jack JH Beck1
2Department of Gynaecology, St. Antonius Hospital Nieuwegein/Utrecht, Netherlands
3Department of Urology, Leiden University Medical Center, Leiden, Netherlands
4Department of Urology, Diakonessenhuis Hospital, Utrecht, Netherlands
5Department of Urology, The Netherlands Cancer Institute-Antoni van Leeuwenhoek Hospital, Amsterdam, Netherlands
Cite this as
Trip EJ, Nicolai MP, Elzevier HW, Pelger RC, Beck JJ (2022) Dutch Sexologist perceptions on monitoring nocturnal erectile function. Int J Sex Reprod Health Care 5(1): 030-034. DOI: 10.17352/ijsrhc.000035Copyright Licence
© 2022 Trip EJ, MD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: There has been a long-standing interest in assessing male sexual function over the past number of decades. Erectile Dysfunction (ED) is commonly classified as organic, psychogenic, or mixed.
Aim: The principal aim of this questionnaire was to determine the ways in which Dutch healthcare professionals (sexologists) define the type of ED in their daily practice. The second aim was to evaluate sexologists’ opinions regarding their experiences with the Rigiscan and the desired aspects of a yet-to-be-developed successor.
Methods: We performed an anonymous survey study. A questionnaire with 21 items was mailed to all participants of the Dutch Association of Sexology. To obtain a higher response rate the survey was sent three times. The questionnaire was designed by two Dutch sexologists from the Sint Antonius Hospital. The survey questions were pre-tested, and after making changes to the questionnaire it was pilot tested.
Outcomes: Eighty-eight people responded and sixty-six respondents completed the survey.
Results: The majority of respondents reported that information obtained by a thorough sexual history, according to the biopsychosocial model, is sufficient to diagnose the cause of ED and enable them to provide the correct therapy. For additional diagnostics, respondents indicate to refer to a urologist for physical examination, basic laboratory tests, or, if necessary, advanced examinations such as a nocturnal penile tumescence measurement. 83% of respondents said to use a simple sensor to differentiate the cause of ED if this would be available. Features respondents mentioned of a future sensor where: validated, patient-friendly, and easy to use at home.
Clinical implications: The data provide information to develop a new sensor to measure nocturnal erections.
Strengths & limitations: Study strengths include: The first report among Dutch sexologists about usage and needs for nocturnal erections measurements. Study limitations include a non-validated questionnaire. A diverse group of Dutch sexologists, not many medical sexologists. Low response rate.
Conclusion: The participating sexologists indicate a need for more clarity regarding the different tools which could be useful for the differentiation between primary organic and primary psychogenic ED. A new validated, patient-friendly sensor that can be used by patients in their home setting was appointed to be helpful.
Introduction
There has been a long-standing interest in the assessment of male sexual function over the past number of decades. Naturally, this interest has typically focused on the evaluation of the erectile response itself [1]. Erectile dysfunction (ED) is the persistent or recurrent inability to attain and maintain an erection sufficient to perform sexual activity [2,3]. The incidence rate of ED (new cases per 1,000 men annually) was 19.2 (mean follow-up of 4.2 years) in a Dutch study [4]. ED is associated with comorbidities such as hypertension, diabetes, pelvic surgery, and lower urinary tract symptoms [5]. The pathophysiology of ED may be vasculogenic, neurogenic, anatomical, hormonal, drug-induced, and/or psychogenic [3,6].
’ED is commonly classified into three groups based on etiology. These include organic, psychogenic, and mixed ED. However, this classification should be used with caution as most cases are actually of mixed etiology. Therefore the use of the term “primary organic” or “primary psychogenic” has been suggested’’ [7].
The diagnosis of ED should include a biopsychosocial description and the score of a validated questionnaire, like the International Index of Erectile Function (IIEF) or the validated shorter version of the Sexual Health Inventory for Men [3]. A focused physical examination is advised for all patients [3]. Additional investigations can be deployed. Further investigations can consist of laboratory blood examination (for example testosterone, prolactin, lipids, and glucose), measuring nocturnal penile tumescence (NPT), duplex ultrasound of penile arteries, arteriography, and dynamic infusion cavernosometry or cavernosography. ED has an effect on physical and psychosocial well-being. ‘ED has progressively emerged as an important sentinel marker of cardiovascular and overall health among men. A timely and accurate diagnosis of ED may thus represent a significant opportunity both to diagnose and treat the dysfunction per se and to identify comorbid and potentially life-threatening conditions’ [8].
In the treatment of ED, the primary goal is to enable the individual or the couple to enjoy a satisfactory sexual experience [3]. In order to achieve this goal, it may sometimes be necessary to demonstrate or exclude a situational ED (psychogenic ED). The present study is focusing on the current use of nocturnal penile tumescence and rigidity measurements with the Rigiscan® [Dacomed Corporation, Minneapolis, Minnesota, USA], first introduced by Bradley in 1985, the Rigiscan is a worldwide valuable diagnostic tool for measuring nocturnal penile erection [9]. The Rigiscan is able to measure the penile circumference and radial rigidity continuously and quantitatively [2]. However, this tool has not been updated since its entrance on the market and it has several disadvantages.
Aim
The primary aim of this study is to determine the ways in which Dutch healthcare professionals (sexologists) define the type of ED in their daily practice. The second aim is to evaluate sexologists’ opinions regarding their experience with the Rigiscan and the desired aspects of the yet to be developed future successor.
Materials and methods
In May 2019 a non-validated questionnaire with 21 items was mailed to all members of the Dutch Association of Sexology (NVVS). The questionnaire consisted of five parts: 1) Demographic data 2) Use of nocturnal erection measurement 3) Usage of nocturnal erection measurements 4) Other options for measuring nocturnal erections 5) Wishes for a new sensor.
The education as a sexologist in the Netherlands is a broad post-academic education for psychologists and doctors and such. The education includes basic knowledge about sexology and has a focus on both medical and psychological sexual problems. It was asked to only continue with the questionnaire if you treat men with erection problems. See Appendix for the translated questionnaire. To obtain a higher response rate, a reminder was sent in June and again in July 2019. The questionnaire was designed by two Dutch sexologists from the Sint Antonius Hospital in collaboration with two urologists from Leiden University Medical Center involved in andrology and sexual health. Unfortunately, there was no validated questionnaire for our research question. This new research question required a specific new instrument. The survey questions were pre-tested in eight individuals similar to the sampling frame to ensure relevancy and consistency in interpretation. After making changes to the questionnaire it was pilot tested.
In order to evaluate how nocturnal erectile function is measured in outpatient practices and what aspects of a measuring device are necessary for the successor of the Rigiscan.
Outcomes were analyzed in IBM SPSS statistics 25. Data were analyzed with the use of descriptive statistics. Descriptive statistics will be given with a mean (standard deviation) or the number of respondents and percentages for these data. The Dutch Medical Ethics Committee was consulted and an application was submitted, but no ethical approval was necessary for this study (registered as W22.029), as it did not meet any of the WHO criteria for clinical research.
Results
The survey was sent to 600 mail addresses on the mailing list of the NVVS. From which 279 messages were read, and 144 respondents opened the hyperlink to the questionnaire. Eighty-eight (15%) persons started the survey and sixty-six respondents (75%) completed the survey. A weighted response rate of 46% (66 out of 144). See Table 1 for the demographic characteristics of the respondents.
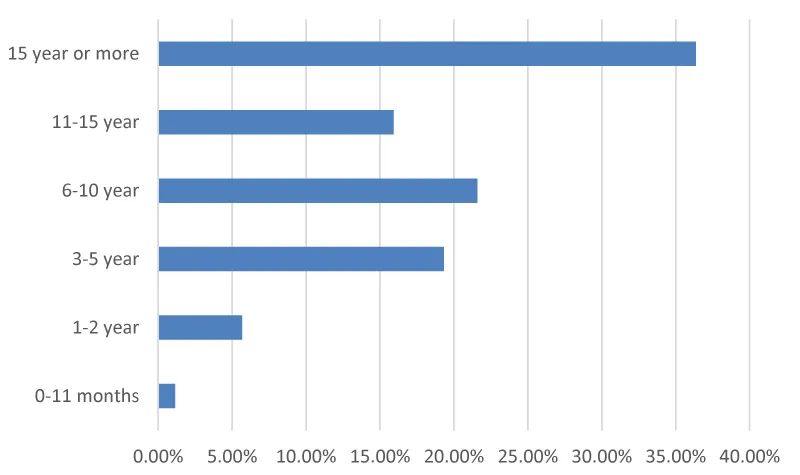
Looking at the respondents, 52% have more than 10 years of experience in sexology. See Figure 1 for the respondent’s complete experience in sexology. Most respondents are female (74%). A great number of 53 out of 88 respondents have no medical education, these respondents are psychologists, nurses, social workers, and physical therapists, all with training in sexology.
Most Dutch sexologists use their anamnesis to discriminate between organic or psychological ED. A majority of 82% indicated using the presence of morning erections to exclude a psychogenic cause. (Question 8).
Only a minority of 23% of the respondents use nocturnal erection measurements in their practices. On the question: “Which measuring instrument do you use for nocturnal erection?” eight people (9%) answered to let their patients perform the stamp test. And 10 people (11%) made use of Rigiscan® to measure nocturnal erections. Two (3%) people don’t measure nocturnal erections but perform a Waking Erectile Assessment (WEA).
The answer to the major advantages of the current measurement method was for sexologists that it was reliable, the gold standard, its simplicity, cheap instrument, and a non-invasive measurement. To the question: ”What do you think are the biggest drawbacks of the current measurement method?” (Question 11) The biggest disadvantage mentioned was the unreliability of test results. Sexologists that did not test for nocturnal erections answered to focus on a detailed description of the biopsychosocial system and extended anamnesis (like the presence of nocturnal and morning erections).
Two respondents performed a WEA and two used blood examinations to differentiate between organic vs psychogenic ED. Most respondents refer to a urologist or a general practitioner for more extensive testing in case this was deemed necessary. 8.6% (6/70) of respondents answered not to test for nocturnal erections at all because of a small number of patients with ED in their clinic. A minority (5.7%) did not know any nocturnal erectile diagnostic tests.
Seventy respondents answered the question: “Why don’t you use a nocturnal erection measurement?” That they are not a physician or nurses, so they will refer patients with ED to a urologist or general practitioner if they think further research is needed to determine the cause of ED. Less than half of the respondents 28 (40%) said not to be in need of diagnostic tests to differentiate between the different categories of ED, because they can be adequately diagnosed with a basic diagnostic workup that includes a comprehensive medical and sexual history, sometimes strengthened with physical examination or laboratory tests. (Question 13) Seven respondents (10%) wrote that NPT was not useful because it’s not a reliable tool.
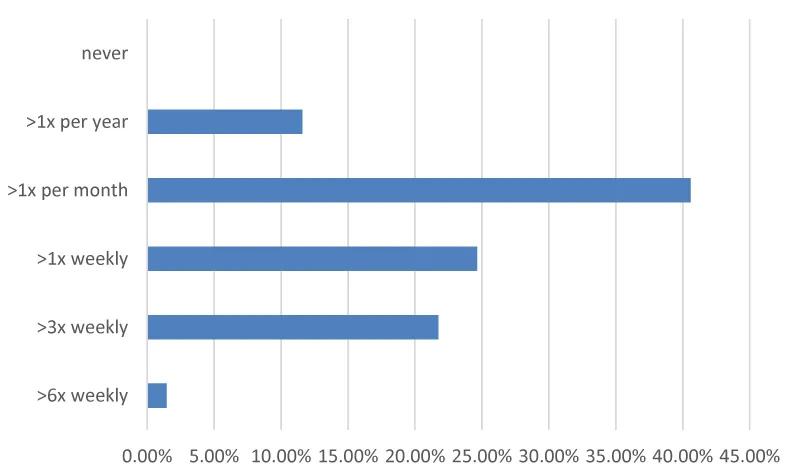
Most of the respondents (83%) noted that they would use a simple sensor to differentiate between organic and psychogenic ED if that would be available. Only 12% (SD18) of patients were referred to a doctor for further investigation into the cause of the erection problems. In 35% (SD 30) of patients, health care professionals would like a nighttime erection measurement if a compact validated sensor was available. And 17% reported not seeing added value from an NPT when a detailed anamnesis is carried out. Most health care professionals see more than one new patient with ED each month (Figure 2).
Respondents were asked to mention conditions that would make a novel sensor useful. The three most mentioned conditions were: validated, patient-friendly, and easy to use at home (Table 2).
Discussion
The present study adds to the current knowledge about the usage of nocturnal erection measurements in sexologists’ daily clinical practice and indicates features important for an improved tool. Only a quarter of sexologists use nocturnal erection measurements in their daily practices. This can be explained by the fact that most respondents are sexologists with a background in psychology and not in medicine. Therefore they do not have nocturnal erections measurement tools at their disposal. When a nocturnal erection measurement was employed the Rigiscan or stamp test is used most often. Some sexologists mentioned that nocturnal erection measurements are unreliable. Indeed, sleep laboratory NPT has been described as the gold standard to distinguish psychogenic from organic ED [1]. Some describe that no investigation we currently use is entirely reliable and no test can be regarded as the gold standard for measuring nocturnal erections [1,10]. In the EAU Guideline the NPTR monitoring is considered as an additional test for even more objectively differentiating between organic and psychogenic ED, ‘but many potential confounding factors may limit its routine use solely for diagnostic purpose’ [7].
Sexologists that indicated not to test nocturnal erections pointed out to focus on a detailed description of the biopsychosocial system and extended anamnesis (like the presence of nocturnal and morning erections). But almost half of the responding sexologists indicated missing an objective diagnostic test to differentiate between the different forms of ED. These respondents indicate they can differentiate forms of ED adequately with a workup that includes a comprehensive medical and sexual history, sometimes strengthened with physical examination or laboratory tests. This argument is not valid, however, as the patient’s recollections of early morning and masturbatory erections are shown to be at best subjective [10]. Although the presence of morning erections is a key factor for excluding a physiological cause, awakening and nocturnal erections occur normally during rapid eye movement (REM) sleep [3]. Sleep disorders therefore can interfere with nightly and morning erections [11]. The presence of nocturnal erections is still the most widely accepted phenomenon to conclude that an organic ED can be excluded from the diagnosis.
This study has several limitations, firstly the response rate was relatively low, although comparable with response rates of other surveys among medical specialists [12,13]. And higher than the average response rate of 30% in emailing questionnaires [14].
In the questionnaire invitation, it was requested only to continue with the questionnaire when regularly treating patients with ED which may have affected the response rate. The gender of respondents was mostly female in accordance with the female/male ratio of the NVVS (78% vs 22%) [15].
The present study is the first reporting results of a survey evaluating European sexologists’ opinions about nocturnal erections measurements. Abdulmohsen et al tested the physicians’ knowledge, attitude, and practice toward ED in Saudi Arabia. It states that the role of physicians is pivotal in diagnosing and treating ED, but the knowledge about ED is below the standard [16]. A minority stated not to know about any nocturnal erectile diagnostic tests. Many sexologists appear to refer to a urologist or general practitioner for more extensive testing if deemed necessary. This is due to a lack of diagnostic possibilities and a lack of knowledge about diagnosing ED. Lack of medical education can be one explanation for not using NPT measurement in the majority of the respondents. Results of this study point to a need for more diagnostic tools that can be used to differentiate forms of ED in daily clinical practice.
‘The current golden standard, the RigiScan, has several drawbacks. First of all, it causes physical discomfort and thereby disturbs natural sleeping patterns. Therefore, results of the measured erections during REM sleep are less reliable’ [17]. Other disadvantages are, for example, lack of updated software, lack of Bluetooth compliance, the enormous size of a simple mechanical sensor, high costs for purchase, maintenance, and disposables, and difficult instructions for both physician and patient [17]. The majority of respondents noted they would use a simple sensor to differentiate between organic and psychogenic ED if available. A new accurate device to differentiate between psychogenic and organic ED is needed in order to treat patients effectively. A new measurement tool that is validated, patient-friendly, used at home, inexpensive, portable, and comfortable would be very welcome. Until now, no accurate sensor that is working simple and is wearable, convenient, and inexpensive is available on the market. This suggests a new device needs to be developed to measure erections.
Conclusion
The results of this study demonstrate the need for more clarity regarding tools to differentiate between primary organic and primary psychogenic ED. A majority indicated using the presence of morning erections to exclude a psychogenic cause. And only a quarter of sexologists use nocturnal erection measurements in their daily practices, the most used for this were the Rigiscan and the stamp test. Furthermore, a new validated, easier-to-use device, replacing the Rigiscan and other tests would be welcomed by sexologists. Research is needed on how patients think about the Rigiscan and what these users see as limitations, and possible improvements.
I would like to acknowledge the NVVS for supporting this questionnaire. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Evelien J. Trip: Conceptualization, Methodology, Formal Analysis, Investigation, Data Curation, Writing – Original Draft and Project Administration.
Melianthe P. Nicolai: Writing - Review & Editing and Supervision
Henk W. Elzevier: Conceptualization, Review & Editing and Supervision
Rob C.M. Pelger: Conceptualization, Review & Editing and Supervision
Jack J.H. Beck: Conceptualization, Writing – Review & Editing and Supervision
Ethical approval: The Dutch Medical Ethics Committee was consulted and an application was submitted, but no ethical approval was necessary for this study (registered as W22.029), as it did not meet any of the WHO criteria for clinical research.
- Qin F, Gao L, Qian S, Fu F, Yang Y, Yuan J. Advantages and limitations of sleep-related erection and rigidity monitoring: a review. Int J Impot Res. 2018 Aug;30(4):192-201. doi: 10.1038/s41443-018-0032-8. Epub 2018 Jun 1. PMID: 29855552.
- Zou Z, Lin H, Zhang Y, Wang R. The Role of Nocturnal Penile Tumescence and Rigidity (NPTR) Monitoring in the Diagnosis of Psychogenic Erectile Dysfunction: A Review. Sex Med Rev. 2019 Jul;7(3):442-454. doi: 10.1016/j.sxmr.2018.10.005. Epub 2019 Jan 4. PMID: 30612976.
- Hackett G, Kirby M, Wylie K, Heald A, Ossei-Gerning N, Edwards D, Muneer A. British Society for Sexual Medicine Guidelines on the Management of Erectile Dysfunction in Men-2017. J Sex Med. 2018 Apr;15(4):430-457. doi: 10.1016/j.jsxm.2018.01.023. Epub 2018 Mar 14. PMID: 29550461.
- Schouten BW, Bosch JL, Bernsen RM, Blanker MH, Thomas S, Bohnen AM. Incidence rates of erectile dysfunction in the Dutch general population. Effects of definition, clinical relevance and duration of follow-up in the Krimpen Study. Int J Impot Res. 2005 Jan-Feb;17(1):58-62. doi: 10.1038/sj.ijir.3901264. PMID: 15510192.
- Braun M, Wassmer G, Klotz T, Reifenrath B, Mathers M, Engelmann U. Epidemiology of erectile dysfunction: results of the 'Cologne Male Survey'. Int J Impot Res. 2000 Dec;12(6):305-11. doi: 10.1038/sj.ijir.3900622. PMID: 11416833.
- Gratzke C, Angulo J, Chitaley K, Dai YT, Kim NN, Paick JS, Simonsen U, Uckert S, Wespes E, Andersson KE, Lue TF, Stief CG. Anatomy, physiology, and pathophysiology of erectile dysfunction. J Sex Med. 2010 Jan;7(1 Pt 2):445-75. doi: 10.1111/j.1743-6109.2009.01624.x. Erratum in: J Sex Med. 2010 Mar;7(3):1316. PMID: 20092448.
- Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, Cocci A, Corona G, Dimitropoulos K, Gül M, Hatzichristodoulou G, Jones TH, Kadioglu A, Martínez Salamanca JI, Milenkovic U, Modgil V, Russo GI, Serefoglu EC, Tharakan T, Verze P, Minhas S; EAU Working Group on Male Sexual and Reproductive Health. European Association of Urology Guidelines on Sexual and Reproductive Health-2021 Update: Male Sexual Dysfunction. Eur Urol. 2021 Sep;80(3):333-357. doi: 10.1016/j.eururo.2021.06.007. Epub 2021 Jun 26. PMID: 34183196.
- Salonia A. Diagnostic Evaluation of a Man Presenting with Erectile Dysfunction. European Urology Supplements. 2013; 12(2): 7–12.
- Zou ZJ, Chen ST, Ma GC, Lai YF, Yang XJ, Feng JR, Zang ZJ, Qi T, Wang B, Ye L, Zhang Y. Consecutive nightly measurements are needed for accurate evaluation of nocturnal erectile capacity when the first-night laboratory recording is abnormal. Asian J Androl. 2020 Jan-Feb;22(1):94-99. doi: 10.4103/aja.aja_40_19. PMID: 31134919; PMCID: PMC6958982.
- McMahon CG, Touma K. Predictive value of patient history and correlation of nocturnal penile tumescence, colour duplex Doppler ultrasonography and dynamic cavernosometry and cavernosography in the evaluation of erectile dysfunction. Int J Impot Res. 1999 Feb;11(1):47-51. doi: 10.1038/sj.ijir.3900369. PMID: 10098954.
- Pressman MR, DiPhillipo MA, Kendrick JI, Conroy K, Fry JM. Problems in the interpretation of nocturnal penile tumescence studies: disruption of sleep by occult sleep disorders. J Urol. 1986 Sep;136(3):595-8. doi: 10.1016/s0022-5347(17)44984-6. PMID: 3735535.
- Nicolai MP, Both S, Liem SS, Pelger RC, Putter H, Schalij MJ, Elzevier HW. Discussing sexual function in the cardiology practice. Clin Res Cardiol. 2013 May;102(5):329-36. doi: 10.1007/s00392-013-0549-2. Epub 2013 Feb 8. PMID: 23392531.
- Krouwel EM, Nicolai MP, van der Wielen GJ, Putter H, Krol AD, Pelger RC, Incrocci L, Elzevier HW. Sexual Concerns after (Pelvic) Radiotherapy: Is There Any Role for the Radiation Oncologist? J Sex Med. 2015 Sep;12(9):1927-39. doi: 10.1111/jsm.12969. PMID: 26381533.
- What’s the average survey response rate? [2021 benchmark]. https://pointerpro.com/blog/average-survey-response-rate/
- https://www.nvvs.info/organisatie/ledenonderzoeken
- Abdulmohsen MF, Abdulrahman IS, Al-Khadra AH, Bahnassy AA, Taha SA, Kamal BA, Al-Rubaish AM, Ai-Elq AH. Physicians' knowledge, attitude and practice towards erectile dysfunction in Saudi Arabia. East Mediterr Health J. 2004 Jul-Sep;10(4-5):648-54. PMID: 16335658.
- Edgar R, Trip EJ, Wolterink GJW, Veltink PH, Beck JJH. New methods for the monitoring of nocturnal erections. Int J Impot Res. 2022 Jan;34(1):1-7. doi: 10.1038/s41443-020-00365-9. Epub 2020 Oct 21. PMID: 33087873.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
